What's the Difference Between
Liver Disease and Cirrhosis?
It can be difficult to distinguish between liver disease and cirrhosis because many of the symptoms overlap, but knowing a bit more about how each condition is classified, can help further understand the distinctions between them.
Liver Disease
Liver disease is broadly classified as one of many conditions that can damage your liver and the essential functions it performs. Over time, untreated or unmanaged liver disease can lead to scarring and more serious complications.
Several factors contribute to liver damage including:
• infections • use of certain medications • alcohol ingestion • poor diet
• blocked or damaged tubes that carry bile from the liver to the intestines
• exposure to toxic chemicals and more
• infections
• use of certain medications
• alcohol ingestion
• poor diet
• blocked or damaged tubes that carry bile from the liver to the intestines
• exposure to toxic chemicals and more
There are many kinds of liver diseases and conditions. The most common include:
Alcohol-Associated Liver Disease (ALD) A result of drinking too much alcohol
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) Often caused by obesity, insulin resistance or imbalance of lipids in the blood, MASLD can progress to Metabolic Dysfunction-Associated Steatohepatitis (MASH) if liver inflammation develops.
Hepatitis Inflammation of the liver caused by viruses (most commonly classified as A, B, or C)
Liver Cancer When cells in the liver grow out of control
Download this FAQ to help answer your questions about liver disease.
Cirrhosis
Living with liver disease or a liver injury for a long time can lead to cirrhosis. Cirrhosis occurs when healthy, normal liver tissue is replaced with scar tissue due to persistent swelling and inflammation of the liver.
Often, a cirrhosis diagnosis can indicate permanent damage to the liver. If not treated, the liver can fail and interrupt functions necessary for daily life including the ability to remove harmful toxins from the blood.
There are many ways cirrhosis can occur in people with liver damage or disease. Common causes of cirrhosis include:
Metabolic-Associated Steatohepatitis (MASH)
A severe form of NAFLD in which the liver becomes inflamed and damaged.
Chronic Viral Hepatitis
Long-term inflammation of the liver caused by a hepatitis virus.
Chronic Alcohol Use Disorder
Long-term severe abuse or misuse of alcohol.
Bile Duct Disease
When bile ducts become damaged, bile can back up into the liver, causing damage to liver cells.
Some Genetic Diseases
Certain inherited conditions can cause toxic substances to build up and damage the liver (i.e., Wilson's disease, cystic fibrosis)
The Role of Portal Hypertension
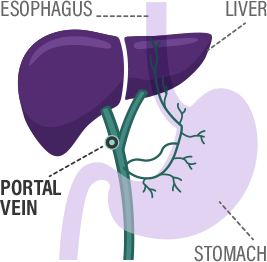
In addition to other changes in liver function, cirrhosis also disrupts the normal flow of blood through the liver. This disruption can lead to a condition called portal hypertension, an increase in pressure in the vein that carries blood from the digestive organs to the liver. This pressure forces blood to bypass the liver through alternative pathways, causing more unfiltered blood and toxins to reach the brain. Over time, portal hypertension can further contribute to the development and progression of HE.

Liver Disease and Cirrhosis can lead to HE
As the liver becomes damaged from liver disease, it can no longer properly clean the toxins from the blood. Once these toxins travel through the body and reach the brain, Hepatic Encephalopathy (HE) symptoms may develop.
Learn more about HE, how it develops, and how to manage the disease.

Liver Disease and Cirrhosis can lead to HE
As the liver becomes damaged from liver disease, it can no longer properly clean the toxins from the blood. Once these toxins travel through the body and reach the brain, Hepatic Encephalopathy (HE) symptoms may develop.
Learn more about HE, how it develops, and how to manage the disease.
LEARN MORE ABOUT HE DETECTIONHow is Hepatic Encephalopathy (HE) Diagnosed?
Diagnosing HE can sometimes be tricky, especially in the early stages when symptoms are subtle. This is why it’s important to recognize and share any changes in your thinking, memory, or behavior with your healthcare provider.
Your healthcare provider may use a combination of the following to diagnose HE:
Talking openly about your symptoms: You’ll be asked about changes like confusion, difficulty concentrating, or mood swings.
Brain function tests: Simple tests may be done to check your memory, attention, and thinking skills.
Blood tests: These can check for toxins, such as ammonia, that build up when the liver isn’t working well. While ammonia levels alone are not a strong indicator of HE, it's important to get blood tests to check for toxins that build up in your blood when the liver is damaged, such as in cirrhosis.
Ruling out other causes: Your doctor will make sure your symptoms aren’t caused by something else, like an infection or medication side effects.
Recognizing the Symptoms
Knowing the symptoms of liver disease and cirrhosis is key to your liver health management. Click here to complete our interactive HE symptom tracker.
In many cases, liver disease often goes unnoticed until it has severely progressed. If symptoms do occur, they may include:
- Loss of appetite
- Nausea or vomiting
- Abdominal pain and swelling
- Tendency to bruise easily
Early symptoms include:
- Fatigue and loss of energy
- Poor appetite and weight loss
- Nausea or belly pain
- Small, red spider-like blood vessels on the skin
As liver function worsens, symptoms may include:
- Fluid buildup in the legs (edema) and in the abdomen (ascites)
- Yellow color in the skin, mucous membranes or eyes (jaundice)
- Redness on the palms of the hands
- Easy bruising and abnormal bleeding, most often from swollen veins in the digestive tract
- Confusion or problems thinking
- Pale or clay-colored stools
- Bleeding from upper or lower intestinal tract
*This list does not represent all possible liver disease symptoms. Make sure to talk to your healthcare provider about any symptoms you may be experiencing that may or may not be associated with liver disease.

Ways to Support Your Liver Health
While it is possible to slow the progression of your liver disease, cirrhosis is not reversible. Having frequent and consistent conversations with your healthcare provider about your symptoms, lifestyle, and overall health is key to assessing your risks for liver disease.
Explore Tools for Early Detection
Some common tips for liver health include:
-

Adopting a healthy lifestyle
Maintaining a healthy weight and exercising -

Liver disease screenings and blood panel tests
Non-invasive screening tests, such as the FIB-4 index, help determine if a patient may have liver damage (fibrosis) and, if measured repeatedly, can help tell if the damage is progressing. This may require further testing or follow-up by a specialist. In adults over age 35, The FIB-4 test uses basic blood test information combined with the age of the patient to calculate a risk score.
Try the FIB-4 Calculator -

Optimizing care for conditions that can lead to liver disease
Regularly seeing your healthcare provider and notifying them if any symptoms of liver disease or cirrhosis occur
If you have liver disease, it is important to follow the care instructions given to you by your healthcare provider to optimize your care plan. It is also important to include your support system throughout your care journey. This will help maintain your health, reduce your risk for chronic liver disease or cirrhosis, and ensure you receive the proper care you may need.

Ways to Support Your Liver Health
While it is possible to slow the progression of your liver disease, cirrhosis is not reversible. Having frequent and consistent conversations with your healthcare provider about your symptoms, lifestyle, and overall health is key to assessing your risks for liver disease.
Explore Tools for Early Detection
Some common tips for liver health include:
-

Adopting a healthy lifestyle
Maintaining a healthy weight and exercising -

Liver disease screenings and blood panel tests
Non-invasive screening tests, such as the FIB-4 index, help determine if a patient may have liver damage (fibrosis) and, if measured repeatedly, can help tell if the damage is progressing. This may require further testing or follow-up by a specialist. In adults over age 35, The FIB-4 test uses basic blood test information combined with the age of the patient to calculate a risk score.
Try the FIB-4 Calculator -

Optimizing care for conditions that can lead to liver disease
Regularly seeing your healthcare provider and notifying them if any symptoms of liver disease or cirrhosis occur
If you have liver disease, it is important to follow the care instructions given to you by your healthcare provider to optimize your care plan. It is also important to include your support system throughout your care journey. This will help maintain your health, reduce your risk for chronic liver disease or cirrhosis, and ensure you receive the proper care you may need.
Resources
If you or a loved one has been diagnosed with liver disease or HE, you may have some additional questions. Get more information about preventing liver disease and managing HE.
.